WP_Post Object
(
[ID] => 3943
[post_author] => 2
[post_date] => 2022-03-07 12:11:51
[post_date_gmt] => 2022-03-07 12:11:51
[post_content] =>
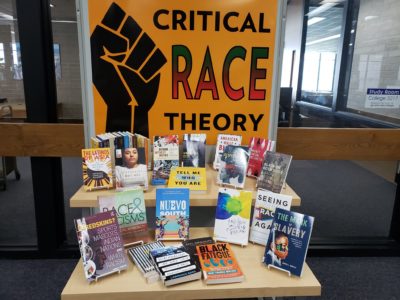
Critical Race Theory has become a Trojan horse for discussions about privilege, gender, race, and inequity, and serves as a rally point for conservative politics.
As the debate over Critical Race Theory, also known as CRT, rages across the United States, the foundational principles, values, and aims of the American education system are called into question. The war over CRT amplifies these essential questions: Who gets to tell the stories of this country, whose stories are worth telling, and how do these stories inform our lives today? It is ironic, of course, that these heated controversies are playing out across historic and contemporary Indigenous homelands.
There is a manufactured nature to the controversy surrounding Critical Race Theory. Far from an attempt to make white children feel guilty about atrocities that took place before they were born, or shame for their skin color, as CRT detractors have argued, the scholars who pioneered and practice the theory use it as a tool for understanding systemic oppression.
Academics recognized CRT in 1989, but its roots go back to the 1960s and 1970s, when legal scholars developed critical legal theory as a means of interrogating how the legal system served the interests of the rich and powerful at the cost of the poor and marginalized. Today, teachers use CRT to inform their age-appropriate lessons about discrimination, history, and oppression. Political pundits who claim that teaching the perspective of the marginalized is the same as teaching CRT are simply wrong.
It’s easy to see how the sudden outrage from right-wing politicians over CRT has deflected attention from this moment of racial reckoning in the post-George Floyd era. Virginia’s Governor Glenn Youngkin, for instance, made opposition to Critical Race Theory a centerpiece of his election campaign; on this platform, he successfully secured his place as Virginia’s first Republican governor in more than a decade. On his first day in office Youngkin made good on his campaign promise by passing an executive order to “end the use of inherent divisive concepts, including Critical Race Theory, and restore excellence in K-12 public education in the commonwealth. Put simply, Critical Race Theory has become a Trojan horse for discussions about privilege, gender, race, and inequity, and serves as a rally point for conservative politics.
To understand the implications of this political development for Native communities, it is important to consider the larger context of Indigenous peoples within existing school curricula. Long before Critical Race Theory was ever formulated, schools in the U.S. failed abysmally in teaching about Indigenous histories, cultures, and contemporary politics. The effect of this failure is painfully obvious among the college students who sit in lecture halls like the ones in which I teach.
As a university faculty member who teaches both American Studies and Native American and Indigenous Studies at a predominately white institution, I often poll students about their knowledge of Native American history and culture, in order to teach effectively. In most cases, their exposure to Native histories is limited to a sanitized version of Columbus’ “discovery” of America, the Thanksgiving myth, and a little bit about the Cherokee Trail of Tears. My students from California often report on their fourth-grade experience of learning about the Spanish mission system—a system of mass death, forced labor, disease, and starvation—by building miniature replicas of the missions out of popsicle sticks and sugarcoating the historical narrative with actual sugar cubes, which they fashioned into mission fixtures.
One of the most striking and disturbing trends I have noticed throughout my years in the classroom and as a public advocate for Indigenous issues is that non-Natives tend to be woefully unaware of the fact that, in addition to the local, state, and federal government levels, there is also the tribal government level. My students are often dismayed to learn that these tribal governments are not marginal, but numerous and powerful—that there are, in fact, 574 sovereign nations with a government-to-government relationship with the federal U.S. governing institutions. The syllabus of my public high school’s civics and government course did not include any lessons about tribal nationhood, self-governance, citizenship, and sovereignty, and this is clearly the case for the vast majority of public schools.
I am deeply concerned to see that our nation’s rising college-educated youth could potentially embark on careers in government without learning that more than 56.2 million acres of this country—for context, only 11 of the 50 states are larger than 56.2 million acres—are under the jurisdiction of tribal governments. Nor are they aware that the largest tribal reservation, governed by the Navajo Nation, is larger than one-fifth of all states, including West Virginia, Maryland, Hawaii, Massachusetts, Vermont, New Hampshire, New Jersey, Connecticut, Delaware, and Rhode Island.
This ignorance is not the fault of the students. The responsibility for ensuring that our youth—our next generation of leaders—receive a historically accurate education and are prepared to go out into the world with a toolbox of knowledge that will carry us all through to the next day falls upon parents, teachers, administrators, and policymakers. At a time when Native students are still subjected to racial slurs, nonconsensual haircutting, Indian-themed mascots, and screeching, headdressed mockeries in their schools, the idea that states are passing legislation that will result in teaching even less essential information about Indigenous peoples and our roles in this nation is extremely difficult to accept or understand.
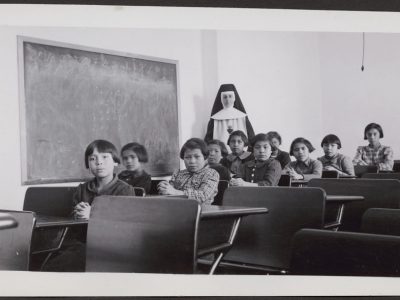
Given the pitiful state of existing education regarding the First Americans, it seems that Critical Race Theory has become the Right’s latest desperate effort to perpetrate a colorblind national narrative. For Native peoples, colorblindness—although not conceptualized as such at the time—can be seen in the pedagogical philosophy of Richard Henry Pratt, the former military officer who, after the Civil War, established residential schools for Native Americans where the guiding pedagogical theory was “kill the Indian, save the man”—i.e., strip Native children forcibly of their culture and language and force them to assimilate into white society.
Pratt ushered in a new policy era that shifted the country’s policies regarding Indigenous populations away from military warfare and physical death, to the new goal of achieving Indigenous cultural and political death through assimilation. Pratt’s Carlisle Indian Industrial School, and hundreds of others that copied his pedagogical model, achieved this aim by separating Indian children from their families and enrolling them in institutions where the children’s hair was cut, their languages and religions forbidden, and all forms of Indigenous community connections disallowed. These are now the sites where hundreds of Native children’s bodies are being discovered in unmarked graves. They are a stain on our national history, an example of the failures of colorblind and assimilationist ideologies, and, indeed, a testament to soundness of the concept of structural racism.
When it comes to the intersection of the current Critical Race Theory debate and Indigenous populations, these continued attempts to silence discussions about the violence endured by Native communities, our strength and resilience in overcoming attempts to wholly eradicate us, and ongoing injustices facing Native peoples today can all be understood within the framework of the attempted erasure our people. But these efforts are not new; various political attempts to “solve” the “Indian problem” have changed and evolved since the founding of the United States.
Those who oppose teaching accurate, representative lessons about Indigenous peoples overlook a fundamental truth that must be reckoned with if we are to continue to grow as a society: Native peoples did not vanish, we are not extinct, and we remain an important part of America’s history and present day. The same is true for Black and other people of color, members of the LGBTQ2S+ community, folks of differing abilities, women, and gender nonconforming individuals, all of whom are represented within the Native population and with whom Indigenous communities are allied in this shared struggle. The very fact that a sizable portion of this nation supports the imposition of legal restrictions on teaching students about race, identity, and history demonstrates the importance of this type of educational instruction.
[post_title] => Critical Race Theory, Native communities, and American education
[post_excerpt] => Critical Race Theory has become a Trojan horse for discussions about privilege, gender, race, and inequity, and serves as a rally point for conservative politics.
[post_status] => publish
[comment_status] => closed
[ping_status] => open
[post_password] =>
[post_name] => critical-race-theory-native-communities-and-american-education
[to_ping] =>
[pinged] =>
[post_modified] => 2024-08-28 21:14:02
[post_modified_gmt] => 2024-08-28 21:14:02
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://conversationalist.org/?p=3943
[menu_order] => 133
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)








 Hazal Sipahi, host of the podcast "Mental Klitoris."[/caption]
When she was a child growing up in provincial Turkey, Sipahi said, sexuality was only discussed in whispers; but as soon as she could speak English, she found an ocean of sexuality content available on the internet.
“I searched for information online and found it, only because I was curious,” she said. “I also learned many false things on the internet, and they were very hard to correct later on.”
For example, Sipahi explained, “For so long, we thought that the hymen was a literal veil like a membrane.” In Turkey there is a widespread belief that once the hymen is “deformed,” a woman’s femininity is damaged, and she somehow becomes less valuable as a future spouse.
“Mental Klitoris” is both Sipahi’s public service and her means of self-expression. She uses her podcast to correct misunderstandings and disinformation, to go beyond censorship and to translate new terminology into Turkish.
“I really wish I had been able to access this kind of information when I was around 14 or 15,” she said.
More than 45,000 people listen to Mental Klitoris, which provides them with access to crucial information in their native tongue. They learn terms like “stealthing,” “pegging,” “abortion,” “consent,” “vulva,” “menstruation,” and “slut-shaming.” Sipahi covers all these topics on her podcast; she says she’s adding important new vocabulary to the Turkish vernacular.
She’s also adding a liberal voice to the ongoing discussion about feminism, “Which became even stronger in Turkey after #MeToo.” She believes her program will lead to a wave of similar content in Turkey.
“This will go beyond podcasts,” she said. “We will have a sexual opening overall on the internet.”
Inspired by contemporary creatives like Lena Dunham (“Girls”), Michaela Coel (“I Might Detroy You”),
Hazal Sipahi, host of the podcast "Mental Klitoris."[/caption]
When she was a child growing up in provincial Turkey, Sipahi said, sexuality was only discussed in whispers; but as soon as she could speak English, she found an ocean of sexuality content available on the internet.
“I searched for information online and found it, only because I was curious,” she said. “I also learned many false things on the internet, and they were very hard to correct later on.”
For example, Sipahi explained, “For so long, we thought that the hymen was a literal veil like a membrane.” In Turkey there is a widespread belief that once the hymen is “deformed,” a woman’s femininity is damaged, and she somehow becomes less valuable as a future spouse.
“Mental Klitoris” is both Sipahi’s public service and her means of self-expression. She uses her podcast to correct misunderstandings and disinformation, to go beyond censorship and to translate new terminology into Turkish.
“I really wish I had been able to access this kind of information when I was around 14 or 15,” she said.
More than 45,000 people listen to Mental Klitoris, which provides them with access to crucial information in their native tongue. They learn terms like “stealthing,” “pegging,” “abortion,” “consent,” “vulva,” “menstruation,” and “slut-shaming.” Sipahi covers all these topics on her podcast; she says she’s adding important new vocabulary to the Turkish vernacular.
She’s also adding a liberal voice to the ongoing discussion about feminism, “Which became even stronger in Turkey after #MeToo.” She believes her program will lead to a wave of similar content in Turkey.
“This will go beyond podcasts,” she said. “We will have a sexual opening overall on the internet.”
Inspired by contemporary creatives like Lena Dunham (“Girls”), Michaela Coel (“I Might Detroy You”),  Tuluğ Özlü[/caption]
Asked to describe how she feels when she crosses the barriers created by widely shared social taboos about human sexuality, Özlü, who lives in Istanbul’s hip
Tuluğ Özlü[/caption]
Asked to describe how she feels when she crosses the barriers created by widely shared social taboos about human sexuality, Özlü, who lives in Istanbul’s hip  Rayka Kumru[/caption]
Kumru said one of the current barriers to freedom in Turkey was the lack of access to comprehensive sexuality education, information and skills such as sex-positivity, critical thinking around values and diversity, and communication about consent. She circumvents that barrier by informing her viewers and listeners about them directly.
“Once connections and a collaborations are established between policy, education, and [particularly sexual] health, and when access to education and to shame-free, culturally specific, scientific, and empowering skills training are allowed, we see that these barriers are removed,” Kumru explains. Otherwise, she says, the same myths and taboos continue to play out, making misinformation, disinformation, taboos, and shame ever-more toxic.
Rayka Kumru[/caption]
Kumru said one of the current barriers to freedom in Turkey was the lack of access to comprehensive sexuality education, information and skills such as sex-positivity, critical thinking around values and diversity, and communication about consent. She circumvents that barrier by informing her viewers and listeners about them directly.
“Once connections and a collaborations are established between policy, education, and [particularly sexual] health, and when access to education and to shame-free, culturally specific, scientific, and empowering skills training are allowed, we see that these barriers are removed,” Kumru explains. Otherwise, she says, the same myths and taboos continue to play out, making misinformation, disinformation, taboos, and shame ever-more toxic. Şükran Moral[/caption]
When it comes to female sexuality, Moral said, Turkey’s art scene is still conservative. “There’s self-censorship among not only creators, but also viewers and buyers, so it’s a vicious cycle.”
Part being an artist, particularly one who challenges the position of women, she said, is seeing a reaction to her work. “When art isn’t displayed,” she asked, “how do you get people to talk about taboos?”
Turkish academia also suffers from a censorship of sex studies.
Dr. Asli Carkoglu, a professor of psychology at Kadir Has University, said it was not easy finding a precise translation for the English word “intimacy” in Turkish.
“There’s the word ‘mahrem,’” she said, but that term has religious connotations.
The difficulty in interpretation, she explains, illustrates the problem: In Turkey, intimacy has not been normalized.
President Recep Tayyip Erdogan and his conservative Justice and Development Party (AKP) have many times expressed support for gender-based segregation and a conservative lifestyle that protects their interpretation of Muslim values.
Erdogan, who has has been in power since 2003, has his own ways of promoting those values.
“At least three children,” has long been the slogan of Erdogan’s population campaign, as the president implores married couples to expand their families and increase Turkey’s population of 82 million.
“For the government, sex means children, population,” Dr. Carkoglu explained.
Dr. Carkoglu believes that sex education should be left to the family, but “when the government acts as though sexuality is nonexistent, the family doesn’t discuss it. It’s the chicken-and-egg dilemma,” she said.
So, how do you overcome a taboo as deep-rooted as sexuality in Turkey? Carkoglu believes that that the topic will have to be normalized through conversations between friends.
“That’s where the taboo starts to break,” she said. “Speaking with friends [about sexuality] becomes normal, speaking in public becomes normal, and then the system adapts.”
But for many Turks, speaking about sexuality is very difficult.
Berkant, 40, has made a living selling sex toys at his shop in the city of Adana, in southern Turkey, for the past two decades. But he said that he’s still too embarrassed to go up to a cashier in another store and say he wants to buy a condom.
“It doesn’t feel right,” he said, adding he doesn’t want to make the cashier uncomfortable.
He is seated comfortably at his desk as we speak; behind him, a wide selection of vibrators are arrayed on shelves.
Berkant and his older brother own one of three erotica shops in Adana. Most of their customers are lower middle class; one-third are female. “Many of them are government workers who come after hearing about us from a friend,” he said.
The shopkeeper said female customers phone in advance to check whether the shop is “available,” meaning empty.
He said he often refers women who describe certain complaints to a gynecologist.
“I see countless women who are barely aware of their own bodies,” he said.
Dr. Doğan Şahin, a psychiatrist and sexual therapist, said that the information women in Turkey hear when they are growing up has a lot to do with their avoidance of discussions about sex, even when the subject concerns their health.
[caption id="attachment_2971" align="aligncenter" width="1600"]
Şükran Moral[/caption]
When it comes to female sexuality, Moral said, Turkey’s art scene is still conservative. “There’s self-censorship among not only creators, but also viewers and buyers, so it’s a vicious cycle.”
Part being an artist, particularly one who challenges the position of women, she said, is seeing a reaction to her work. “When art isn’t displayed,” she asked, “how do you get people to talk about taboos?”
Turkish academia also suffers from a censorship of sex studies.
Dr. Asli Carkoglu, a professor of psychology at Kadir Has University, said it was not easy finding a precise translation for the English word “intimacy” in Turkish.
“There’s the word ‘mahrem,’” she said, but that term has religious connotations.
The difficulty in interpretation, she explains, illustrates the problem: In Turkey, intimacy has not been normalized.
President Recep Tayyip Erdogan and his conservative Justice and Development Party (AKP) have many times expressed support for gender-based segregation and a conservative lifestyle that protects their interpretation of Muslim values.
Erdogan, who has has been in power since 2003, has his own ways of promoting those values.
“At least three children,” has long been the slogan of Erdogan’s population campaign, as the president implores married couples to expand their families and increase Turkey’s population of 82 million.
“For the government, sex means children, population,” Dr. Carkoglu explained.
Dr. Carkoglu believes that sex education should be left to the family, but “when the government acts as though sexuality is nonexistent, the family doesn’t discuss it. It’s the chicken-and-egg dilemma,” she said.
So, how do you overcome a taboo as deep-rooted as sexuality in Turkey? Carkoglu believes that that the topic will have to be normalized through conversations between friends.
“That’s where the taboo starts to break,” she said. “Speaking with friends [about sexuality] becomes normal, speaking in public becomes normal, and then the system adapts.”
But for many Turks, speaking about sexuality is very difficult.
Berkant, 40, has made a living selling sex toys at his shop in the city of Adana, in southern Turkey, for the past two decades. But he said that he’s still too embarrassed to go up to a cashier in another store and say he wants to buy a condom.
“It doesn’t feel right,” he said, adding he doesn’t want to make the cashier uncomfortable.
He is seated comfortably at his desk as we speak; behind him, a wide selection of vibrators are arrayed on shelves.
Berkant and his older brother own one of three erotica shops in Adana. Most of their customers are lower middle class; one-third are female. “Many of them are government workers who come after hearing about us from a friend,” he said.
The shopkeeper said female customers phone in advance to check whether the shop is “available,” meaning empty.
He said he often refers women who describe certain complaints to a gynecologist.
“I see countless women who are barely aware of their own bodies,” he said.
Dr. Doğan Şahin, a psychiatrist and sexual therapist, said that the information women in Turkey hear when they are growing up has a lot to do with their avoidance of discussions about sex, even when the subject concerns their health.
[caption id="attachment_2971" align="aligncenter" width="1600"] Advertisement for men's underwear in Izmir, Turkey.[/caption]
Men don’t really care whether the woman is aroused, willing or having an orgasm, he said. Unless the problem is due to pain, or vaginismus, couples rarely head to a therapist, he adds.
“[Women who grew up hearing false myths] tend to take sexuality as something bad happening to their bodies, and so, they unintentionally shut their vaginas, leading to vaginismus. This is actually a defense method,” he told The Conversationalist.
“They fear dying, they fear becoming a lower quality woman, or that sex is their duty.”
While most Turkish women find out about their sexual needs after getting married, the doctor says that, based on research he completed about 10 years ago, men tend to fall for myths about sexuality by watching pornography, which plants unrealistic fantasies about sex in their minds.
“Sexuality is also presented as criminal or banned in [Turkish] television shows. The shows take sexuality to be part of cheating, damaging passions or crimes instead of part of a normal, healthy, and happy life.”
He recommends that couples talk about sexuality and normalize it. Talking is crucial, and so is the language used in those conversations.
Bahar Aldanmaz, a Turkish sociologist studying for her PhD at Boston University, told The Conversationalist why talking about menstruation matters.
“A woman’s period is unfortunately seen as something to be ashamed of, something to be hidden,” she said. (According to Turkey’s language authority, the word “dirty” also means “a woman having her period.”)
“There are many children who can’t share their menstruation experience, or can’t even understand they are having their periods, or who experience this with fear and trauma.”
And this is what builds a wall of taboo around this essential issue, the professor says. It is one of the issues her non-profit organization “We Need To Talk” aims to accomplish, among other problems related to menstruation, such as period poverty and period stigma.
Female hygiene products are taxed as much as 18 percent—the same ratio as diamonds, said Ms. Aldanmaz. She adds that this is what mainly causes inequality—privileged access to basic health goods, the consequence of the roles imposed by Turkish social mores.
“Despite declining income due to the COVID-19 pandemic, there is a serious increase in the pricing of hygiene pads and tampons. This worsens period poverty,” Aldanmaz says. She offers Scotland as an example of what would like to see in Turkey: free sanitary products for all.
During Turkey’s government-imposed lockdown in May 2021, several photos showing tampons and pads in the non-essential sales part of markets stirred heated debates around the subject, but neither the Ministry of Family and Social Services nor the Health Ministry weighed in.
“We are fighting this shaming culture in Turkey,” Aldanmaz says, “by understanding and talking about it.”
[post_title] => Sexually aware and on air: Beyond Turkey's comfort zone
[post_excerpt] => Turkish podcasts that host frank conversations about sexuality are smashing taboos and filling information vacuums.
[post_status] => publish
[comment_status] => closed
[ping_status] => open
[post_password] =>
[post_name] => sexually-aware-and-on-air-beyond-turkeys-comfort-zone
[to_ping] =>
[pinged] =>
[post_modified] => 2024-08-28 21:14:02
[post_modified_gmt] => 2024-08-28 21:14:02
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://conversationalist.org/?p=2949
[menu_order] => 187
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
Advertisement for men's underwear in Izmir, Turkey.[/caption]
Men don’t really care whether the woman is aroused, willing or having an orgasm, he said. Unless the problem is due to pain, or vaginismus, couples rarely head to a therapist, he adds.
“[Women who grew up hearing false myths] tend to take sexuality as something bad happening to their bodies, and so, they unintentionally shut their vaginas, leading to vaginismus. This is actually a defense method,” he told The Conversationalist.
“They fear dying, they fear becoming a lower quality woman, or that sex is their duty.”
While most Turkish women find out about their sexual needs after getting married, the doctor says that, based on research he completed about 10 years ago, men tend to fall for myths about sexuality by watching pornography, which plants unrealistic fantasies about sex in their minds.
“Sexuality is also presented as criminal or banned in [Turkish] television shows. The shows take sexuality to be part of cheating, damaging passions or crimes instead of part of a normal, healthy, and happy life.”
He recommends that couples talk about sexuality and normalize it. Talking is crucial, and so is the language used in those conversations.
Bahar Aldanmaz, a Turkish sociologist studying for her PhD at Boston University, told The Conversationalist why talking about menstruation matters.
“A woman’s period is unfortunately seen as something to be ashamed of, something to be hidden,” she said. (According to Turkey’s language authority, the word “dirty” also means “a woman having her period.”)
“There are many children who can’t share their menstruation experience, or can’t even understand they are having their periods, or who experience this with fear and trauma.”
And this is what builds a wall of taboo around this essential issue, the professor says. It is one of the issues her non-profit organization “We Need To Talk” aims to accomplish, among other problems related to menstruation, such as period poverty and period stigma.
Female hygiene products are taxed as much as 18 percent—the same ratio as diamonds, said Ms. Aldanmaz. She adds that this is what mainly causes inequality—privileged access to basic health goods, the consequence of the roles imposed by Turkish social mores.
“Despite declining income due to the COVID-19 pandemic, there is a serious increase in the pricing of hygiene pads and tampons. This worsens period poverty,” Aldanmaz says. She offers Scotland as an example of what would like to see in Turkey: free sanitary products for all.
During Turkey’s government-imposed lockdown in May 2021, several photos showing tampons and pads in the non-essential sales part of markets stirred heated debates around the subject, but neither the Ministry of Family and Social Services nor the Health Ministry weighed in.
“We are fighting this shaming culture in Turkey,” Aldanmaz says, “by understanding and talking about it.”
[post_title] => Sexually aware and on air: Beyond Turkey's comfort zone
[post_excerpt] => Turkish podcasts that host frank conversations about sexuality are smashing taboos and filling information vacuums.
[post_status] => publish
[comment_status] => closed
[ping_status] => open
[post_password] =>
[post_name] => sexually-aware-and-on-air-beyond-turkeys-comfort-zone
[to_ping] =>
[pinged] =>
[post_modified] => 2024-08-28 21:14:02
[post_modified_gmt] => 2024-08-28 21:14:02
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://conversationalist.org/?p=2949
[menu_order] => 187
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)




 Working as a pediatric emergency physician, Dr. Shaheen-Hussain saw the cruel consequences of the non-accompaniment practice first-hand in 2017, when he treated two young patients who were undergoing stressful medical procedures without their loved ones by their side. Quebec pediatricians had been demanding the end of this heartless practice for decades, but successive governments refused to change the policy, making Quebec an outlier in Canada. When a citizen confronted him about the matter at a public event in 2018 , Quebec’s then-Health Minister, Gaétan Barrette,
Working as a pediatric emergency physician, Dr. Shaheen-Hussain saw the cruel consequences of the non-accompaniment practice first-hand in 2017, when he treated two young patients who were undergoing stressful medical procedures without their loved ones by their side. Quebec pediatricians had been demanding the end of this heartless practice for decades, but successive governments refused to change the policy, making Quebec an outlier in Canada. When a citizen confronted him about the matter at a public event in 2018 , Quebec’s then-Health Minister, Gaétan Barrette, 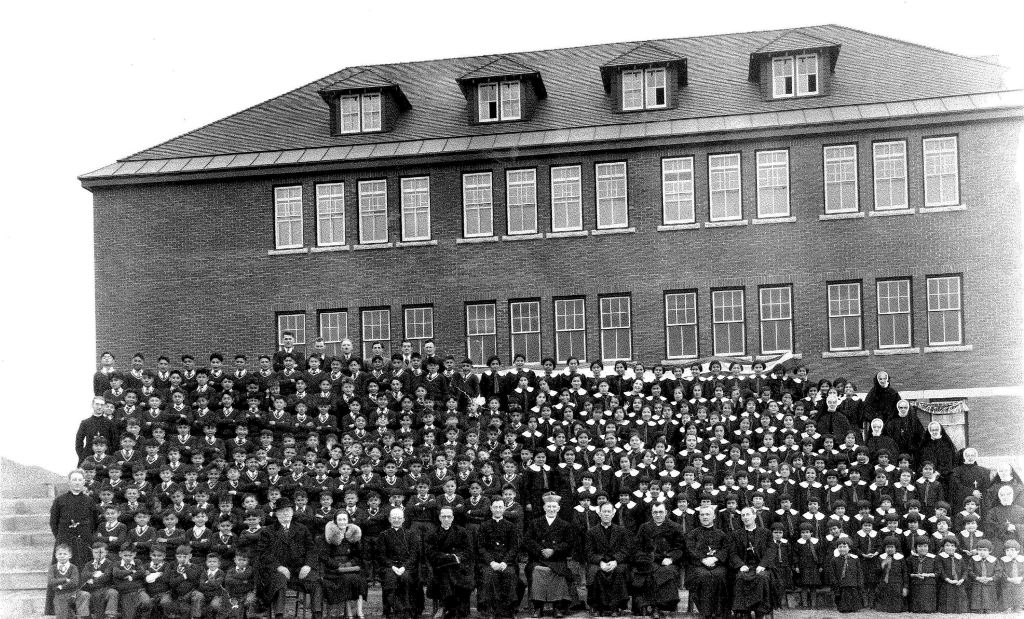 Kamloops Indian Residential School in 1937.[/caption]
In addition, highly unethical
Kamloops Indian Residential School in 1937.[/caption]
In addition, highly unethical  A Black man is tested during the Tuskegee Study of Untreated Syphilis in the Negro Male.[/caption]
The
A Black man is tested during the Tuskegee Study of Untreated Syphilis in the Negro Male.[/caption]
The