Government inquiries have exposed Canada’s systemic racism toward Indigenous people.
In September 2020, Joyce Echaquan, a 37-year-old Atikamekw woman from Quebec’s Manawan community, livestreamed a Facebook video that showed her screaming in pain while hospital healthcare workers openly mocked her. “You’re a fucking idiot,” “only good for sleeping around,” and “you are better off dead,” were just some of the comments recorded. Joyce passed away shortly after posting the video, which was shared widely online; the collective shock and shame at her death galvanized a movement to force Canadians to come to terms with the racism and colonialism in their medical system.
During the public inquiry that followed, witnesses and hospital staff testified to long-standing prejudice from healthcare workers and hospital administrators who neither knew nor cared that Indigenous patients were receiving inadequate care. Advocates for First Nations communities pointed to this incident not as an isolated tragedy, but as one more example of a medical system that continues to see Indigenous peoples as less deserving of equal treatment and respect.
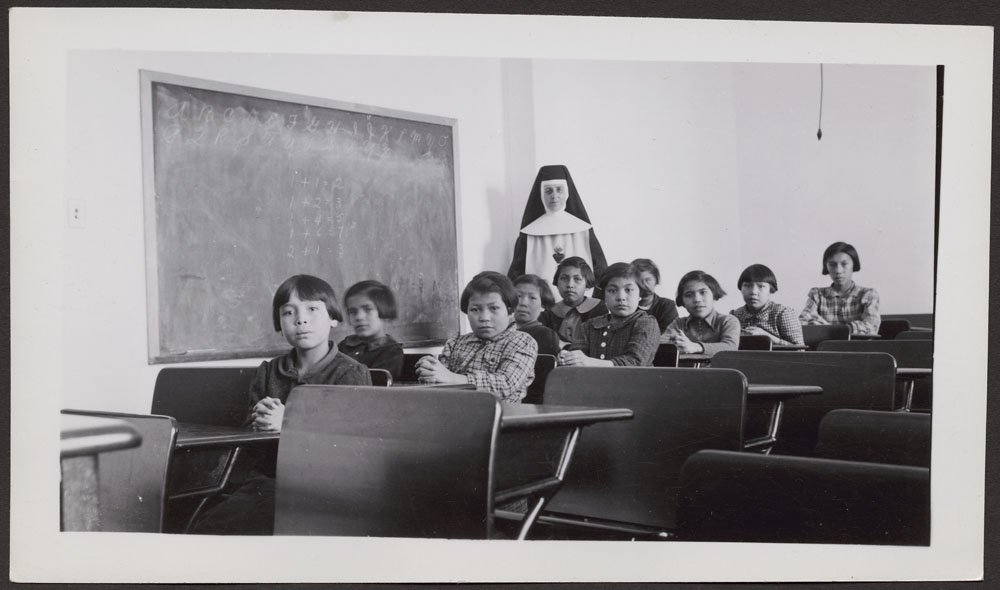
A culture of anti-Indigenous racism
Among those testifying at the inquiry was Dr. Samir Shaheen-Hussain, an assistant professor in the Faculty of Medicine at McGill University and a Montreal pediatric emergency physician, who spoke about medical colonialism as “a culture or ideology, rooted in systemic anti-Indigenous racism, that uses medical practices and policies to establish, maintain or advance a genocidal colonial project.”
While not many people are familiar with the term, Dr. Shaheen-Hussain has written a book on the subject. Fighting for a Hand to Hold: Confronting Medical Colonialism against Indigenous Children in Canada (2020, McGill-Queens University Press) shines a light on the decades-long cruel practice of separating children from their families during emergency medevacs from northern and remote regions of Quebec.
Working as a pediatric emergency physician, Dr. Shaheen-Hussain saw the cruel consequences of the non-accompaniment practice first-hand in 2017, when he treated two young patients who were undergoing stressful medical procedures without their loved ones by their side. Quebec pediatricians had been demanding the end of this heartless practice for decades, but successive governments refused to change the policy, making Quebec an outlier in Canada. When a citizen confronted him about the matter at a public event in 2018 , Quebec’s then-Health Minister, Gaétan Barrette, made comments that basically amounted to propagating “drunken Indian” and “freeloader” tropes. Calls for his resignation went unheeded, but the practice of preventing parents from accompanying their children on medevac flights was finally discontinued later that year, on the back of a campaign called #aHand2Hold.
Confronting the truth of past horrors
The same week that Dr. Shaheen-Hussain testified at the Quebec inquiry on Echaquan’s death a grim discovery on the other side of the country, in Kamloops, British Columbia, stopped Canadians in their tracks. A mass grave containing the remains of 215 Indigenous children at the site of a former residential school provided physical confirmation of what thousands of survivors of these forced-assimilation centres had been saying for years.
In 2015, the Truth and Reconciliation Commission (TRC) a nationwide commission on the evils of these government-sponsored, church-run schools that operated between 1831 and 1996, concluded that thousands of children had been mistreated, physically and sexually abused, and knowingly left vulnerable to outbreaks of disease, resulting in thousands of deaths.
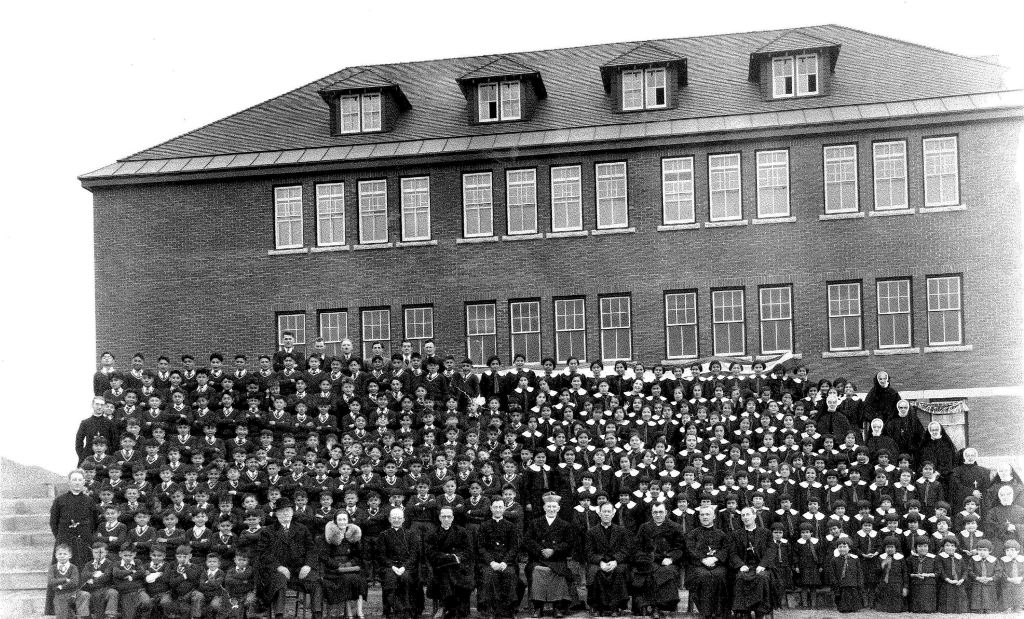
In addition, highly unethical nutrition experiments under the care of two physicians (one of them was a former president of the Canadian Paediatric Society and one of three inventors of Pablum infant cereal) working for the Department of Indian Affairs of Canada had been conducted on many of these children without their knowledge or consent. They were purposefully denied adequate nutrition or dental care, as part of these experiments, eerily reminiscent of the Syphilis Study conducted on Black men by the U.S. Public Health Service at Tuskegee and the medical experiments Nazi doctors performed on concentration camp survivors during World War II. Even when children died, the experiments continued.

The TRC commission made a number of recommendations, among them a request for the federal government to “acknowledge that the current state of Aboriginal health in Canada is a direct result of previous Canadian government policies, including residential schools” and to “establish measurable goals to identify and close the health outcomes between Aboriginals and non-Aboriginal communities […] via efforts [that] would focus on indicators such as: infant mortality, maternal health, suicide, mental health, addictions, life expectancy, birth rates, infant and child health issues, chronic diseases, illness and injury incidence, and the availability of appropriate health services.” Out of a total of 94 recommendations or calls to action made in 2105, only eight have since been implemented.
A lack of compassion and respect
Dr. Arlene Laliberté, a psychologist who is Algonquin from the Timiskaming First Nation, completed her PhD on suicide in Indigenous communities. She sees the effects of medical colonialism and the intergenerational and multigenerational trauma caused by the residential school and child welfare systems (often manifesting as structural violence and self harm) daily in her work. She also sees the indifference to it.
“Collaboration and communication are always difficult with hospitals and healthcare institutions,” she says. “When I accompany patients of mine who are going through crises or mental health issues, I often observe a lack of compassion, a lack of understanding, an unwillingness to follow up with the patient or the patients’ family. They aren’t taken seriously or believed when they disclose symptoms, and their pain is minimized or dismissed.”
Dr. Laliberté says that Indigenous patients are often treated as second-class citizens, with no respect for their own traditional healing methods, not being seen beyond the stigma or cliches of being “a bunch of drunks” and “savages.” As a result they tend to mistrust the system or delay treatment for serious physical or mental health issues, often until it’s too late.
Attempting to bridge this ignorance gap, the TRC commission called upon medical and nursing schools in Canada to require all students take a course dealing with Aboriginal health issues, including the history and legacy of residential schools, the United Nations Declaration on the Rights of Indigenous Peoples, Treaties and Aboriginal rights, and Indigenous teachings and practices. According to the commission, this would require “skills-based training in intercultural competency, conflict resolution, human rights, and anti-racism.”
“As far as I know, this still isn’t part of the curriculum,” says Dr. Laliberté. “While I was teaching at the university, I thought of how overrepresented Indigenous children are in the foster care system (a whopping 52.2 per cent of children in foster care in Canada are Indigenous, although they account for only 7.7 percent of the child population), and I took it upon myself to educate future psycho-educators who will be working in the DPJ (Quebec’s Youth Protection system). Some of my peers voiced strong opposition to this and weren’t interested in anything that wasn’t part of the status quo.”
Forced sterilization of Indigenous women
Unwanted medical procedures are not only part of our colonial history –they continue to be part of the present. This past May, a local Métis (person of mixed Indigenous and European ancestry) lawyer in British Columbia alleged that he knew of Indigenous girls— some younger than 10 years old—who had been forced by social workers to have IUDs inserted by doctors because they were at risk of being raped in foster care.
These disturbing allegations came on the heels of the final report of the National Inquiry on Missing and Murdered Indigenous Women and Girls (MMIWG), which included a section on the forced sterilization of Indigenous Women in Canada. It reminds us that commonplace medical procedures are often used without consent to decrease or limit the Indigenous population.
There are parallels here with similar coercive sterilization tactics implemented in the United States. The Family Planning Services and Population Research Act of 1970 enabled the mass sterilization (some say more than 25 percent) of Native American women of child-bearing age. Back in Canada, the province of Saskatchewan is currently facing a class-action lawsuit from women alleging they were coerced into getting tubal ligation as recently as 2014. A similar lawsuit has since been launched in Alberta.
“Medical colonialism killed Joyce”
This colonial mindset and the systemic discrimination that deeply affects issues regarding standards of care, ethics, caregiver policies and practices is often a straight line from the past to today’s medical system, with healthcare staff often making fast and damaging assumptions about Indigenous patients and why they’re seeking medical help. During the inquiry for Echaquan, who died of pulmonary edema, witnesses testified that healthcare staff mistook her debilitating pain and severe myocardiopathy for drug withdrawal symptoms. As a result, they disregarded her cries of pain and left her unmonitored, which was against healthcare protocol. According to the testimony of Dr. Alain Vadeboncoeur, an emergency physician at the Montreal Heart Institute, who examined her autopsy report, the 37-year-old mother of seven “could have been saved with proper care.”
Dr. Shaheen-Hussain shared similar conclusions at the inquiry, stating categorically that “medical colonialism killed Joyce Echaquan and that her death was avoidable.”
Medicine isn’t always healing
Dr. Shaheen-Hussain’s book is a powerful condemnation of medical colonialism, which continues to affect Indigenous communities. The descriptions of forced sterilization, skin grafting, Indian Hospitals (sanatoriums), medical nutritional experiments, and medical disappearances speak loudly to deeply embedded racism in medical culture. No wonder Indigenous communities are suspicious of the Canadian healthcare system and the people who work within it.
“How the government responded to the #AHand2Hold campaign is telling, because if denial stems from the top, one can only imagine what it’s often like on the frontlines,” says Dr. Shaheen-Hussain. “Medical colonialism is rooted in the long-held belief that medicine is benevolent and neutral, but it’s often not, and we need to come to terms with that reality.”
Unconscious bias also manifests in how Indigenous health professionals are perceived by the medical establishment. “We are often seen as less competent,” Dr. Laliberté says. “I didn’t get my PhD in a cracker box, and yet, despite my credentials, I am often seen as less respectable. I have also seen the services offered on a reserve deemed less valuable, even though the registered professionals working there have the same education as everyone else.” The Indian Act and the infantilization of Indigenous peoples as “wards of the state” still unconsciously resonates today with many who should know better.
Joyce’s Principle
After Echaquan’s tragic death, the Atikamekw community drafted Joyce’s Principle, which aims to guarantee all Indigenous people the right of equitable access, without any discrimination, to all social and health services, as well as the right to enjoy the best possible physical, mental, emotional, and spiritual health. The brief constitutes a reminder and a formal request for a commitment by the governments of Quebec and Canada (and their institutions) to respect and protect Indigenous rights relative to healthcare and social services rights that are recognized internationally. The federal government adopted Joyce’s Principle, but the Quebec government refused because the document makes explicit mention of systemic racism, which the provincial government insists does not exist.
Indigenous academics, advocates, physicians, and the Quebec Nurses’ Association (QNA) immediately blasted the government for its stubborn refusal. In a published statement, the QNA said, “Without explicit confirmation of the presence of such problems, little changes or actions will lead to positive results.”
The government’s refusal to adopt Joyce’s Principle is, according to Dr. Shaheen-Hussain, “a slap in the face, unconscionable, insulting, and destructive to Indigenous communities’ idea of working together for a better future.”
He finds the government’s stubborn refusal to acknowledge systemic racism “jarring.” “It’s like trying to provide treatment for a diagnosis you refuse to name,” he says. “This refusal is so perplexing to me, because, contrary to accusations that it puts ‘all Quebecers on trial,’ if you accept systemic racism, you’re actually doing the exact opposite. You’re in fact acknowledging that you’ve inherited a system that you’re simply part of and should be actively working to dismantle.”
Gaslighting government
The minister responsible for Indigenous Affairs in Quebec insists he doesn’t want to get tangled up in semantic debates and prefers to take concrete action. But advocates insist that a government denying precisely what those it seeks to re-establish trust with are asking for is, once again, gaslighting their concerns.
Dr. Shaheen-Hussain makes it clear this isn’t a semantic debate to those affected. “Systemic racism and medical colonialism are why infant mortality is four times higher for Inuit children than average childhood mortality rates in Quebec. It’s why it’s twice as high for Indigenous children ages 10-19 than the Canadian average and five times as high for Indigenous teenage girls living on a reserve. It’s because of an entire system, not because of a few racist people.”
He insists that throwing money at a problem the government isn’t even willing to recognize in any meaningful way is pointless. “There’s no tangible commitment to eradicate systemic racism at its root.”
Quebec’s response is to casually point to the federal government and blame the Indian Act of 1876 for all the ills that have befallen Indigenous communities over the years. This is convenient deflection and denial, according to Dr. Shaheen-Hussain. “There is a fair amount of historical proof that proves the contrary,” he says. “Quebec is complicit in systemic racism and colonialism too.”
First Nations and their best interests are often caught in the middle of a power struggle between both of Canada’s colonizing forces (the English and the French) as the Quebec and federal governments often engage in a push and pull over jurisdictions and territory. When much-needed federal legislation was finally adopted in 2019, allowing Indigenous groups to take over their own child welfare systems, which would prioritize the placement of Indigenous children within their own communities, the Quebec government challenged it because it saw the new legislation as a threat to its provincial jurisdiction. The move understandably angered the Indigenous community, which called it “shameful.”
A complicit medical system
Chronic underfunding of health services and social services and the unwillingness to relinquish power as a way of redressing social inequities is also medical colonialism. Canadian medical anthropologist John O’Neil, who’s briefly mentioned in Dr. Shaheen-Hussain’s book, writes that “the system of medicine that we now rely on not only assisted that [colonial] expansion, but it was assisted in its development and domination by the colonial process of subjugation and resource exploitation.”
In the book’s afterword, Kanesatake activist Ellen Gabriel reveals that in the Mohawk language, the word for “hospital” is Tsi Iakehnheiontahionàhkhwa, which equates to “the place where people go to die.” It’s quite telling that the medical institutions most of us think of as sources of healing and help are seen as a place of death by those who have suffered—and continue to suffer—under them.
For her part, Dr. Laliberté defines medical colonialism as “living in fear and frustration.” She witnesses the daily struggle by Indigenous communities across Canada for respect and empathy, engaged in reclaiming traditional measures that support their peoples’ mental health and wellness, being challenged by a colonial mindset that presumes to know better.
“Living my life as a First Nations professional woman, I am livid most of the time,” she says.